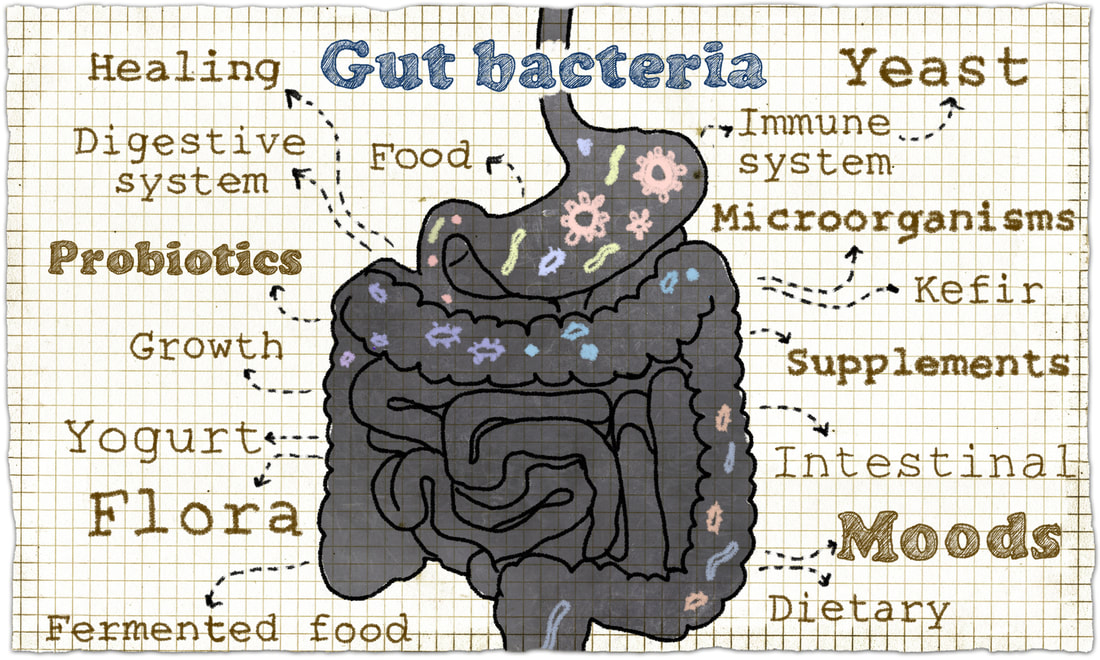
Ronit Mor, NDThe gut is literally the gateway to health. There is no part of the body, no disease, no organ system – that the gut does not directly or indirectly affect. Studies have confirmed that not only does the gut transfer food to vital organs, but it plays a role in our physical health, mental health, emotional stability, immunology, neurology, endocrinology, and pathology. Our Microbiome Are As Unique As Our Fingerprints Our body is, in fact, a complex ecosystem made up of more than 100 trillion microbes (10 times the number of human cells!) that must be properly balanced and cared for if we are to be healthy. If aliens were to take a human body and analyze it cell by cell, they would come to the conclusion that we are mostly a mass of bacteria with just a few human cells mixed in. Collectively, these trillions of bacteria are called the microbiome. Most of those bacteria reside in our gut (the gut microbiota), and they play multiple roles in our overall health. Similar to fingerprints, each of us has a unique combination of types and proportions of gut bacteria. In the past few years, scientists have dedicated millions of research dollars to the investigation of the gut microbiota. As a result, there is growing recognition and evidence demonstrating that our diet and lifestyle impact our health by the influence it has on the balance and vitality of our microbiome. In other words, the state of our microbiome affects not only the integrity of our gut but also autoimmune disease, obesity, and even how well the liver metabolizes alcohol. The Gut-Brain Connection Most of us have become familiar with the term “good” bacteria and the positive role that it plays in digestive health. Science is now beginning to realize how this good bacteria also influences the human brain and the state of a person’s mental and emotional health. The ability of gut bacteria to bi-directionally communicate with the brain, known as the gut-brain axis, thus influencing human health is currently at the forefront of scientific research. There are multiple mechanisms that exist that connect the gut and the brain together – in both directions, in fact. Changes in the gut can affect the brain and changes in the brain can affect the gut. The new model of brain chemistry holds that inflammation in the gut produces inflammation that cross the gut barrier, enters the bloodstream, travels through the blood, crosses the blood-brain barrier, enters the brain and suppresses the activity of the frontal cortex – the part of the brain that deals with higher brain function. Suppression of frontal cortex activity results in all typical signs of depression. This creates a vicious cycle where suppressed activity in the frontal cortex leads to more gut problems because the brain controls the gut. Research confirms that intestinal microbiota influences brain chemistry and behavior independently of the autonomic nervous system, gastrointestinal-specific neurotransmitters, or inflammation. An imbalanced microbiota might contribute to psychiatric disorders in patients with bowel disorders. It is associated with depression, anxiety, and other neurological problems ranging from epilepsy to Parkinson’s disease to autism spectrum disorder. The Gut-Immune System Connection The gut is actually an incredibly important barrier between our body and the outside world. Our gut wall houses 70% of the cells that make up our immune system. Anything inside our gut is technically actually outside our body, with several defenses between it and our bloodstream. That makes our gut a first line of defense. Many conditions such as allergies, arthritis, autoimmune diseases (irritable bowel syndrome, acne, chronic fatigue), mood disorders, autism, dementia and cancer are actually attributed to our gut’s health. The gut microbiota protect against invaders in several ways: they strengthen the physical defenses of the gut wall; they increase the chemical barriers to infection by affecting the pH of the gut environment; they compete with potential pathogens for space and food; they regulate inflammation and the inflammatory immune response; and they produce various antimicrobial substances. For optimal immunity, detoxification and nourishment, our gut must function seamlessly! The Gut-Skin Connection If the eyes are the window to our soul, then the skin could be considered the window to our gut. Our skin is our largest organ, and is a barometer which can be used to monitor internal health. Acne, facial redness, eczema, psoriasis, dry skin, and rosacea are all skin conditions which may have the same root cause: poor gut health. An imbalance in the gut microbiota has been shown to impact the physical, chemical and antimicrobial defense system of our skin. Over a century ago, dermatologists Drs Stokes and Pillsbury linked changes in the gut microbiota to inflammation that can manifest in the skin. They connected bad skin with abnormal levels of stomach acid which, in turn, is connected to SIBO (Small Intestinal Bacterial Overgrowth). SIBO has been shown to cause systemic and local inflammation as well as nutritional deficiencies in vitamins essential for optimal skin health. In short, an imbalance in gut microbiota can impact the amount of inflammation, infection and irritation expressed externally on our skin. The gut’s health is not the cause for all skin conditions; however, it can play a significant role in the severity and aggravation of most skin conditions. Keep Your Microbiota Happy – 8 Practical Tips for Supporting Your Gut
Scientists studying the gut microbiota, suggest that a healthy gut consist of about 80% good to 20% bad bacteria. These levels may dip a bit, but as long as we stay in the majority of this balance, our gut and immune system are able to function most efficiently, and our body overall stays in good health. To improve your gut’s health, you should consider the following:
Comments are closed.
|
Archives
October 2022
Categories
All
|
|
FOLLOW US
|
RESOURCES
|
©2020-2024 Ronit Mor LLC. ALL RIGHTS RESERVED
All statements on this website have not been evaluated by the Food and Drug Administration. The content of this website is not intended to diagnose, treat, cure, or prevent any disease.
All statements on this website have not been evaluated by the Food and Drug Administration. The content of this website is not intended to diagnose, treat, cure, or prevent any disease.

 RSS Feed
RSS Feed